‘Just take some buscopan,’ a doctor told me, with the tone and facial expression of someone that was not only confused why I was complaining but also annoyed that I was wasting her time. It was the second time in as many months that I’d been to the doctors for severe period pains, and the second time I’d left more frustrated than ever. On my third attempt, I was finally prescribed mefenamic acid, a painkiller that actually took my cramps from unbearable to manageable.
I’ve had quite the journey in managing my reproductive health. I went on the pill at 15 because my menstrual cramps were forcing me off school for too much time, and heavy bleeding combined with acne were becoming the bane of my life. After four years on the combined hormone pill, I was taken off it because family history ruled me unsuitable – family history that should have been on my record before I ever started the pill – and moved onto the single hormone (progesterone only) pill. That’s when the pain started again, more severe than before, and this time I was in university, much higher stakes.
After eight months – the amount of time advised to let a new contraceptive settle- of continuous bleeding and cramps that forced me to miss lectures and work, I was advised to try an IUD. Not only would it stop my periods, I was told, it would help my acne, another side effect of taking the progesterone-only pill. Despite also being treated for acne since I was 15, it wasn’t taken into account when putting me on a pill that is known for worsening the skin condition. I conceded that my uterus hates me when the cramps and bleeding continued on the IUD for another 10 months.
It took a year and a half with my IUD before my body properly settled, the cramps subsided and my periods were relatively normal. I guess my womb realised the patriarchy would never allow for a contraceptive that didn’t cause me debilitating pain and gave me a break.
Over the course of four years since coming off the combined pill, I’ve told more than a dozen different health professionals about my severe cramps and bleeding. I’ve heard the words ‘put up with it’ in a dozen different, less blunt ways.
My experience is not rare. In fact, a report by Public Health England revealed this morning that 31% of women experience severe reproductive health problems, but under half seek help. We're told that women are too embarrassed to seek help, with the report stating that ‘stigma surrounding reproductive health was a key concern for women taking part in the survey, with less than half of women seeking help for their symptoms, regardless of severity.’
Stigma around reproductive health is important. With 59% of respondents revealing they’ve lied to their boss about needing time off work for menopause symptoms, there’s clearly an uncomfortable work culture surrounding menstrual health. Everyone should feel comfortable telling their boss they’re in too much pain to work, regardless of why.
However, there’s a difference between women not feeling comfortable telling their boss why they’re off sick, and women not seeking help for severe reproductive health problems. The idea that we’re all too embarrassed to deal with our reproductive health, to attend smear tests, to discuss periods, is ignoring another, bigger problem around how seriously we take women's health issues.
In a 2003 study, published in the Journal of Law, Medicine & Ethics, researchers found that women experience 'more frequent and greater pain' than their male counterparts, but will 'be less well treated than men for their painful symptoms'. And in 2016, Dr. Beth Darnall, a pain psychologist at the Stanford Pain Management Center told The Guardian that she often treats women who've 'seen multiple providers, they’ve been through primary care for their pain, they’ve probably seen another specialist, and then they come to us'.
Not only do women receive less supportive treatment than we need when we do seek treatment, but we're finding it hard just to get through the door in the first place. Last week, Jo’s Cervical Cancer Trust reported that cervical cancer screenings were down by 52%. Not because we’re too embarrassed to get our bits out, but because women are struggling to access the tests thanks to a decline in sexual health services. The £531 million in cuts to public health budgets have left them struggling, now understaffed and overburdened at a time when demand is continuing to rise.
‘An increasing number of people are being turned away from clinics,’ says Karin O'Sullivan, clinical consultant at sexual health charity FPA, ‘This is particularly apparent in London, with one NHS trust reporting turning away 600 people a week from an open-access service and another clinic reporting that 1,500 people were trying to book 300 spots on a daily basis.’
‘But don’t sexual health clinics only treat sexual health problems?’, I hear you ask. While that is meant to be their primary function, according to Karin, reproductive health is part of the parcel they offer.
‘Most sexual health services are now integrated with contraception and reproductive health services and women do access these services for reproductive health issues,’ she continued, ‘this really depends on a number of things such as the area and services available, and the age of the patient. For example, young women and more vulnerable patients are often more likely to attend sexual health services than a GP.’
Alas, with sexual health services declining and demand only rising, women are left with fewer options to treat their reproductive health concerns. And when they are able to receive treatment? They’re met with responses like I’ve received for four years, being told our severe pain is normal and our heavy bleeding will settle if we just give it six to eight months.
So no, we’re not embarrassed, we’re exhausted. Exhausted by a system that takes so much time and effort to access, just to be told our debilitating pain, our endless heavy bleeding, whatever it may be, is normal. It isn’t, and if it is, it shouldn’t be.
But will we have to deal with this for much longer? It seems as if the optimistic answer is no. According to the same report by Public Health England, women’s reproductive health will now be considered ‘a public health issue that needs to be addressed’. Bringing together 18 healthcare bodies, including the Department of Health & Social Care, NHS England and the Royal College of GPs, the PHE is creating ‘an integrated cross-governmental five-year action plan, informed by the best available data and women’s real-life experiences of reproductive health symptoms.’
It’s a hopeful, and long-awaited, development in a society that has historically ignored women’s health concerns. However, whether the action plan will tackle what is necessary to remains to be seen. With a report focusing on the women being embarrassed about reproductive health concerns, we can only hope that the ‘best available data’ also shows a need for change in how many women can assess services, and how their treated when they eventually do. We need more than being able to tell our boss we’re having period pains, we need effective healthcare when that actually happens.
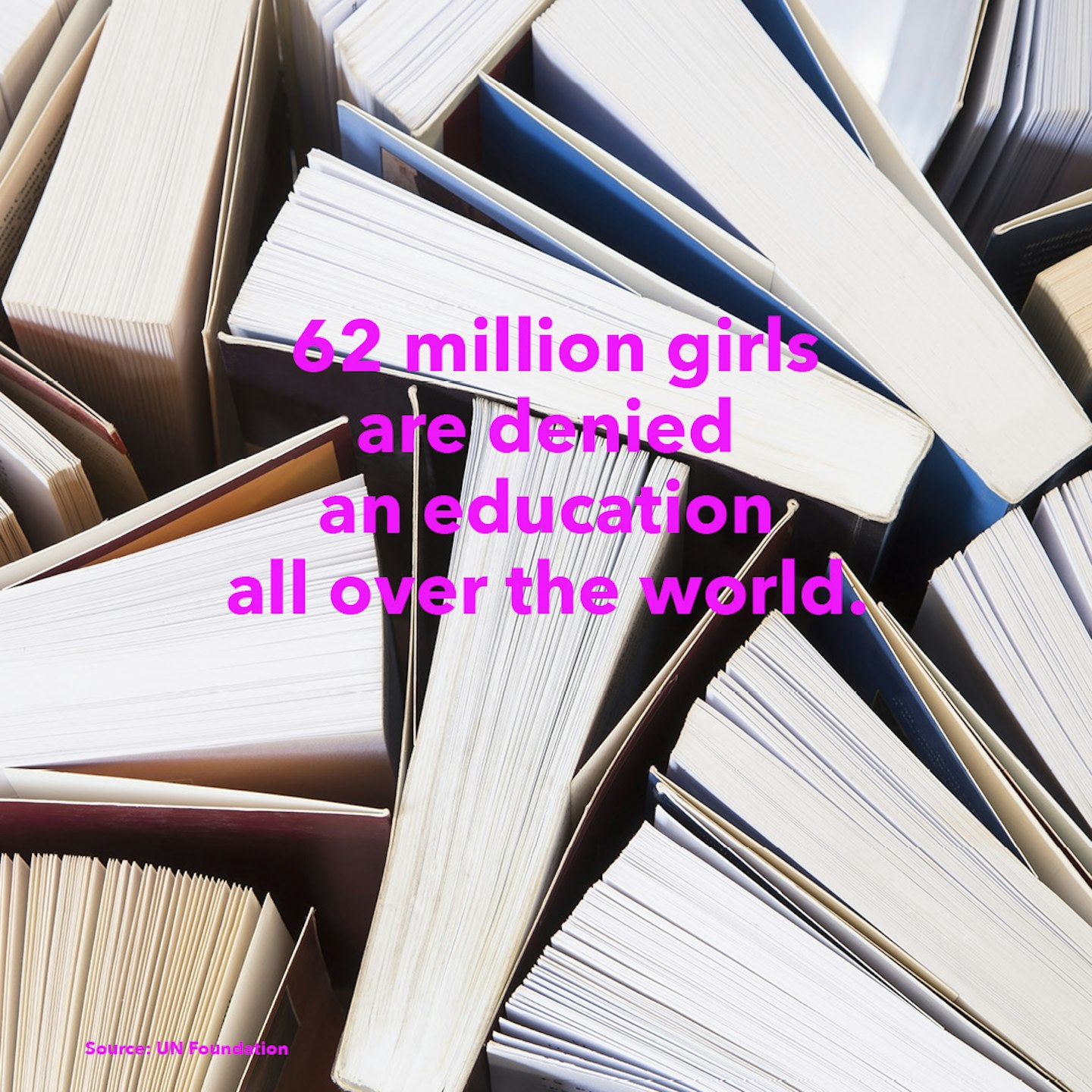
Click through to see facts about sexism around the world...
Debrief Facts about women around the world
 1 of 18
1 of 18Facts about women around the world
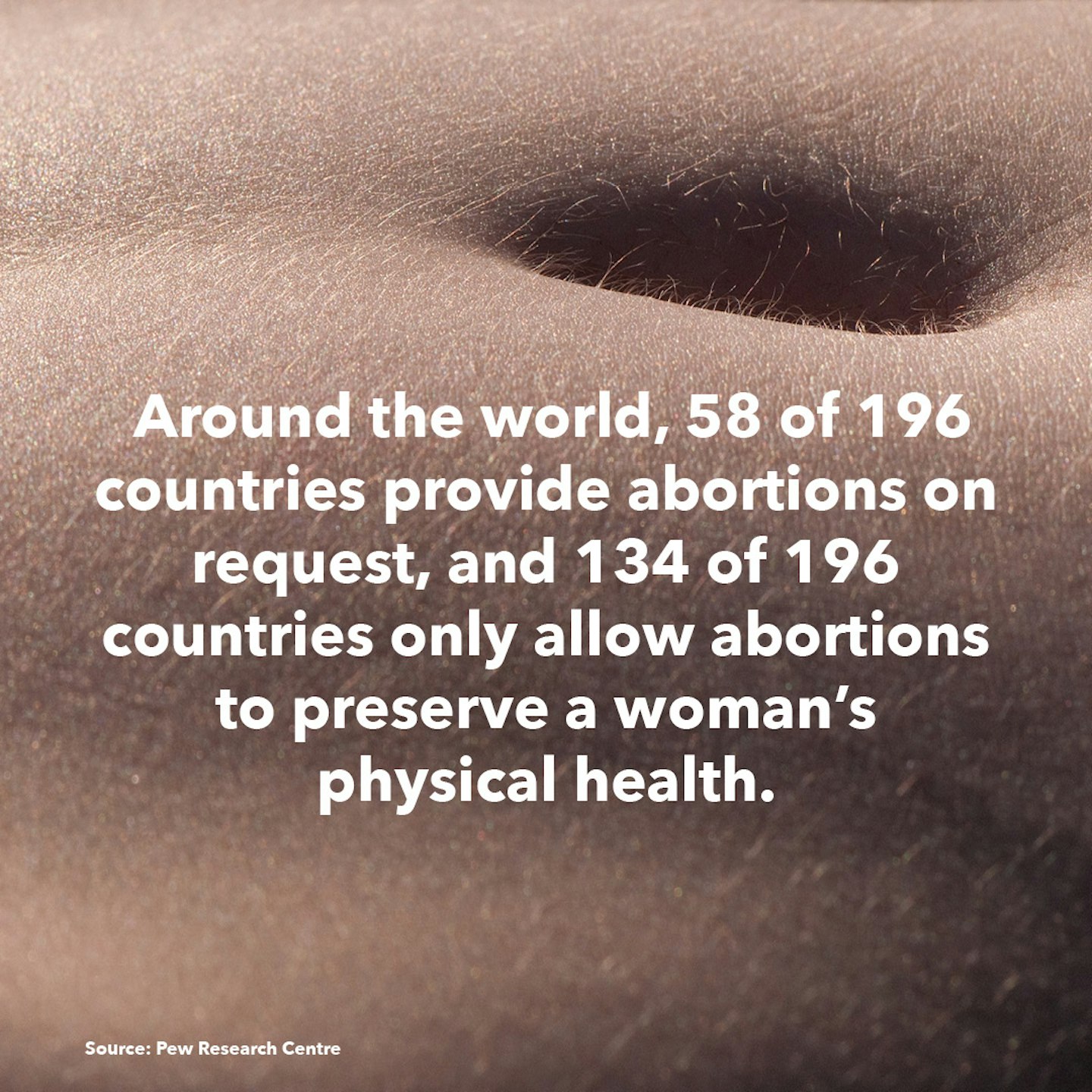
 2 of 18
2 of 18Facts about women around the world
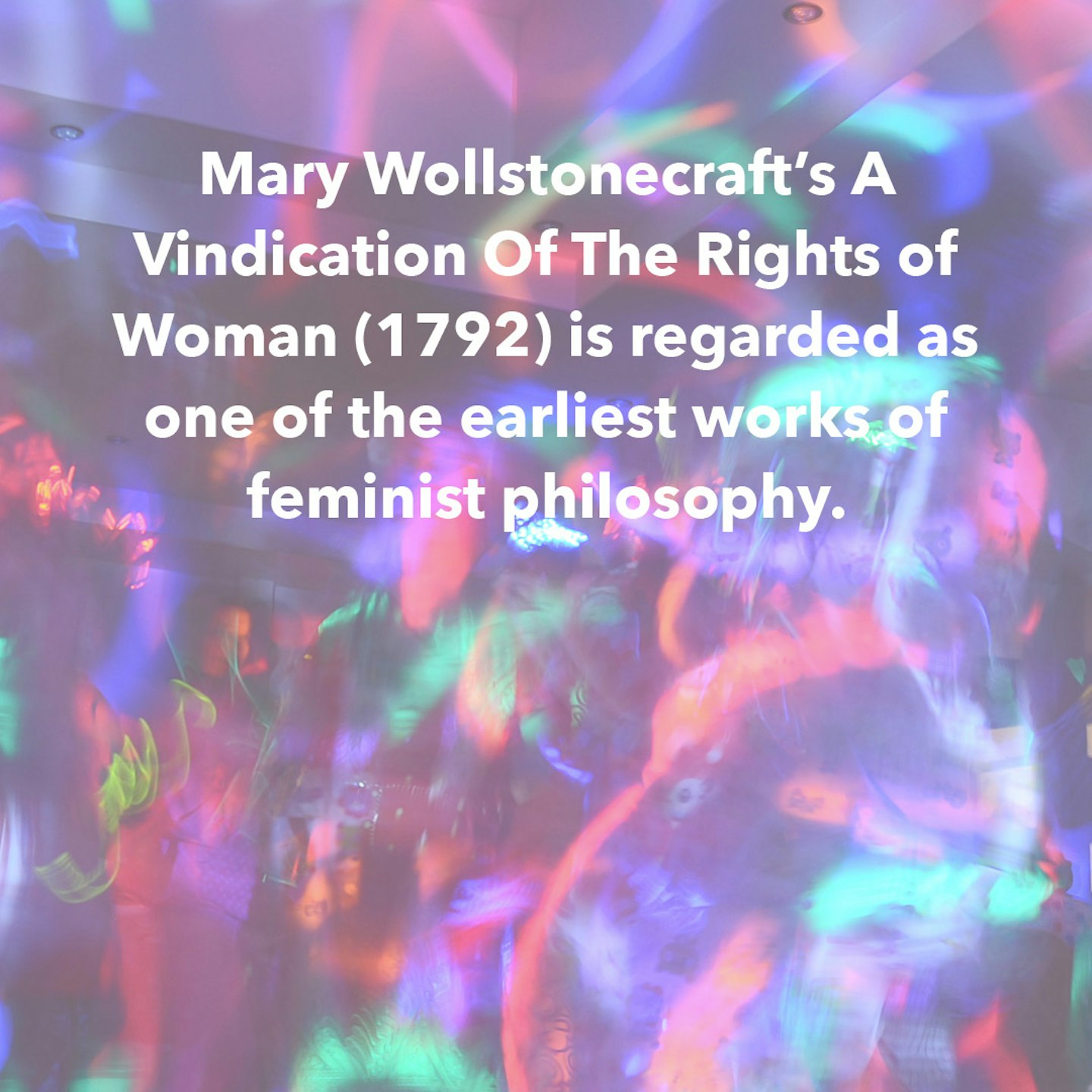
 3 of 18
3 of 18Facts about women around the world
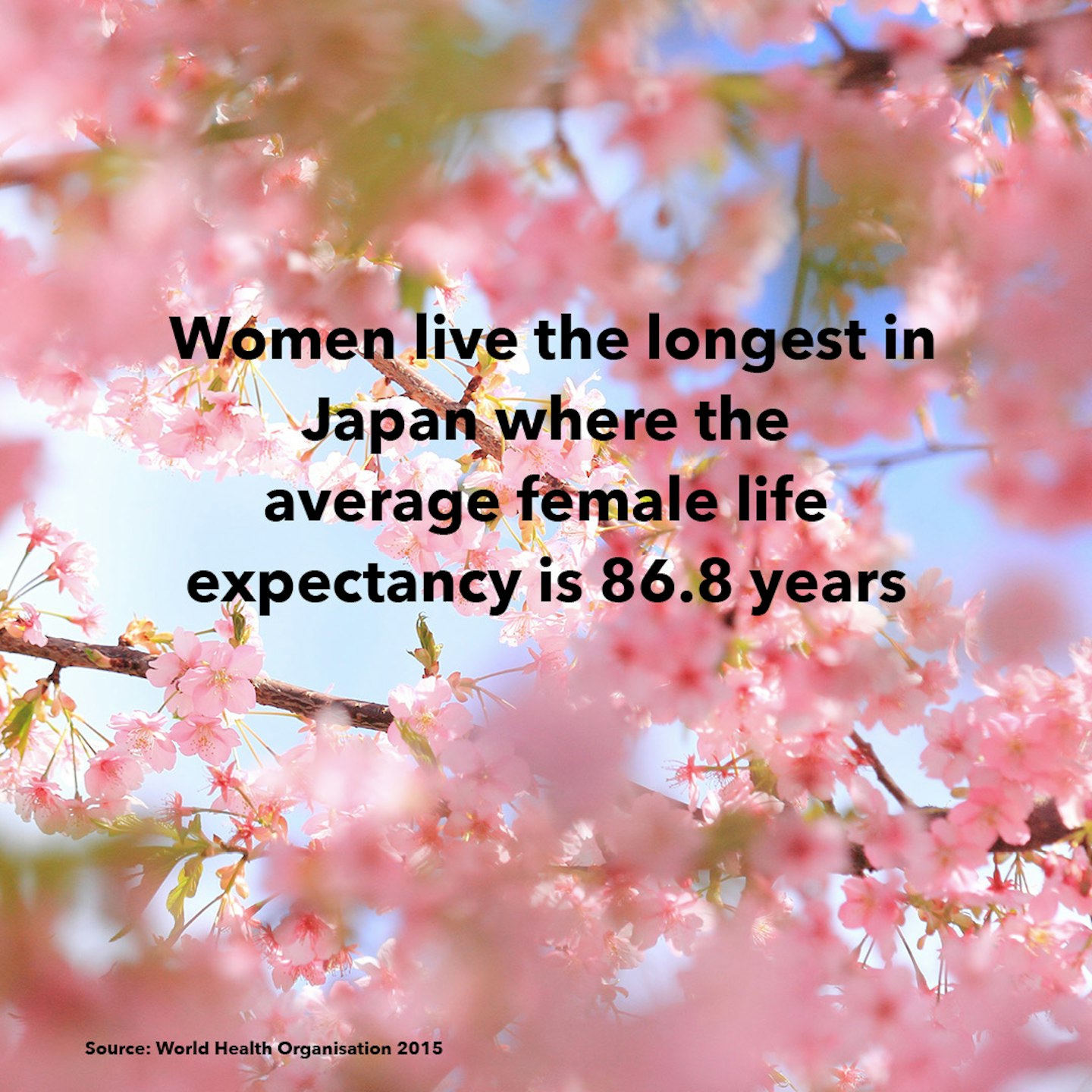
 4 of 18
4 of 18Facts about women around the world
 5 of 18
5 of 18Facts about women around the world
 6 of 18
6 of 18Facts about women around the world
 7 of 18
7 of 18Facts about women around the world
 8 of 18
8 of 18Facts about women around the world
 9 of 18
9 of 18Facts about women around the world
 10 of 18
10 of 18Facts about women around the world
 11 of 18
11 of 18Facts about women around the world
 12 of 18
12 of 18Facts about women around the world
 13 of 18
13 of 18Facts about women around the world
 14 of 18
14 of 18Facts about women around the world
 15 of 18
15 of 18Facts about women around the world
 16 of 18
16 of 18Facts about women around the world
 17 of 18
17 of 18Facts about women around the world
 18 of 18
18 of 18