‘When you are going through fertility treatment you have to try everything you can because you can't live with the guilt that that might have been the factor that made the difference,’ says Catherine Strawbridge, 39, who is currently on her fourth round of IVF treatment after six years of trying to get pregnant.
Having experienced two rounds on theNHS and two privately, Catherine was offered the endometrial scratch procedure on her third cycle of IVF. ‘For round three it was talked about because I’d had miscarriages previously’, she tells me, ’it was expensive, over £300, but when you've been doing this as long as us you have to try everything you can.’
The endometrial scratch is the latest procedure found to have no additional benefit for those undergoing IVF. It involves grazing the tissue lining the womb in an effort to cause inflammation, previously thought to help embryos implant. Similar to a smear test, it essentially involves taking a tissue biopsy and so is painful and invasive.
While previous studies suggested the endometrial scratch benefited IVF by improving the rate of live births, new research, and the most comprehensive to date, has found it does not increase the chances at all. The procedure isn’t routinely offered on the NHS, however private fertility clinics offer it for as much as £350.
Researchers studied 1,364 women across 13 centres and give countries, with half of the women randomly undertaking the procedure and half not. Both groups had the same 26% rate of live births, and there were no differences in the rates of ectopic or multiple pregnancies. In fact, the study also found that there were no benefits for women who had tried IVF multiple times, something the procedure was previously thought to help.
As a result, the senior author of the study, Cindy Farquhar, postgraduate professor of obstetrics and gynaecology at the University of Auckland, has called for clinics to stop offering the procedure.
‘I think it is unreasonable for clinics to ask for patients to pay for something when there is now clear evidence that there is no added benefit,’ she told The Guardian. ‘I would hope that it will disappear from the list of add-ons that many clinics have both in the UK and in New Zealand and Australia.’
For someone like Catherine, not seeing it as an option is the only thing that would stop her from pursuing something that she hadn’t tried before on her IVF journey. ‘Would I do it again in the situation I was in? I would irrelevant of the research,’ she says, ‘rationally you wouldn’t, but emotionally, because of the guilt, you don’t want to have any regrets so you would still do it.’
It’s something that many women who’ve experienced IVF relate to, according to Fertility Network chief executive Aileen Feeney. ‘The danger is, people that are emotionally distressed will take a chance at everything,’ she tells me. ‘Clinics need to point [the endometrial scratch research] out to patients because if its misrepresented in terms of the success rate they get it’s just not right and it’s not fair.’
Whether or not patients will take the advice regardless of research then depends just how rational one can be in such an emotional situation.When patients are expected to make emotionally-driven decisions about their own treatment - and how much money they subsequently spend on it - more research needs to be done to find out exactly what procedures and add-ons are beneficial so clinics can either stop offering them or at the very least give realistic advice.
‘My second round was private and we went to a clinic in Harley Street and we spent over’ £20,000’ she continued, ‘we did a lot of add-ons there.’ And while that might sound like a lot to spend, Catherine insists ‘you find the money’, or as is the case with many women ‘you have to stop because you can’t afford it, and that boils down to the postcode lottery.’
Ultimately, that’s the biggest concern with research such as this coming to light. More and more women are spending thousands privately because they no-longer receive the same level of NHS-funded IVF treatmentas women do in other parts of the country. Not only is it unfair, but when research such as this emerges and shows that actually it could be a wasted expense, it’s yet another kick for women already on this emotionally distressing journey. With NHS services offering IVF continuing to decline, will this problem only continue to worsen?
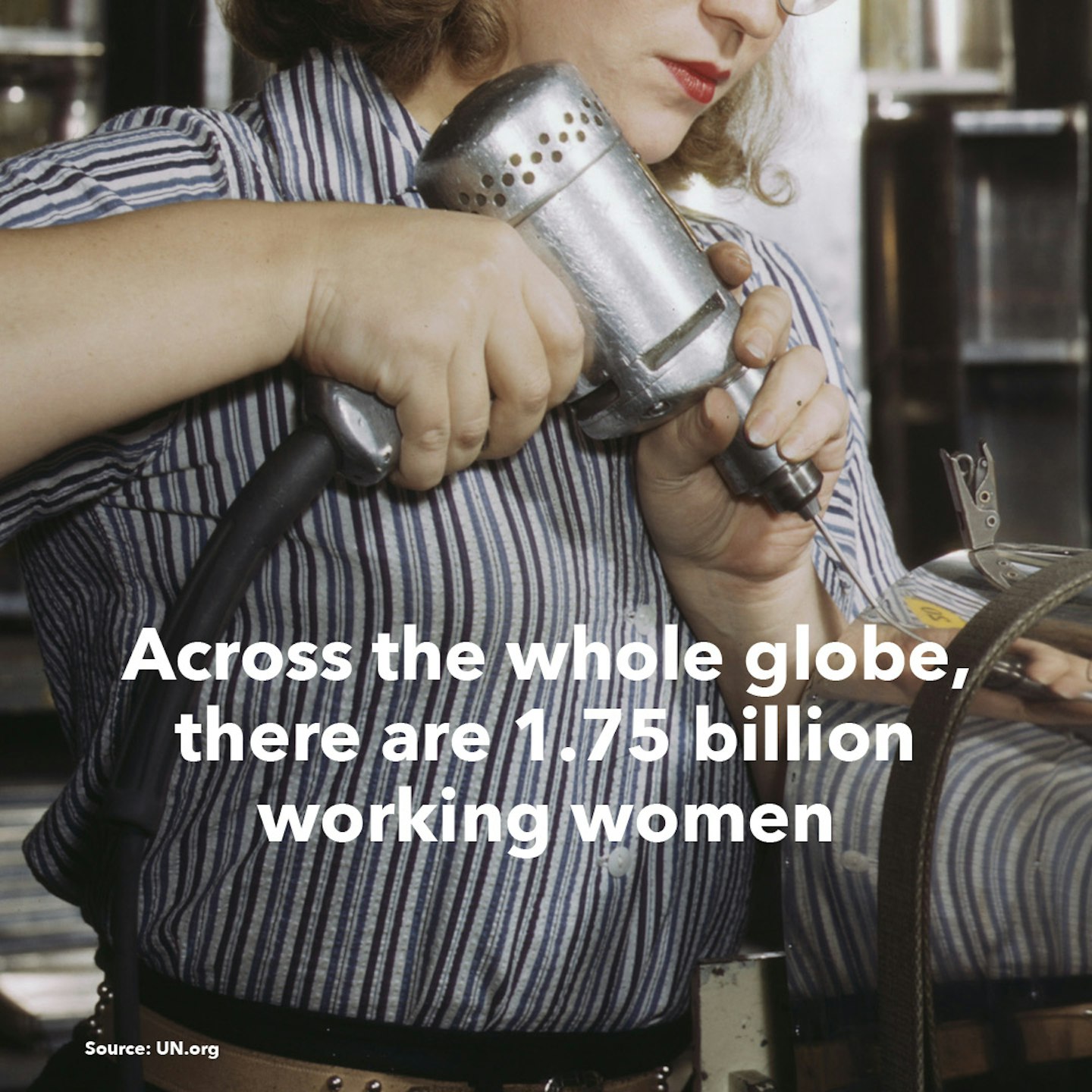
Click through to read facts about women around the world...
Debrief Facts about women around the world
 1 of 18
1 of 18Facts about women around the world
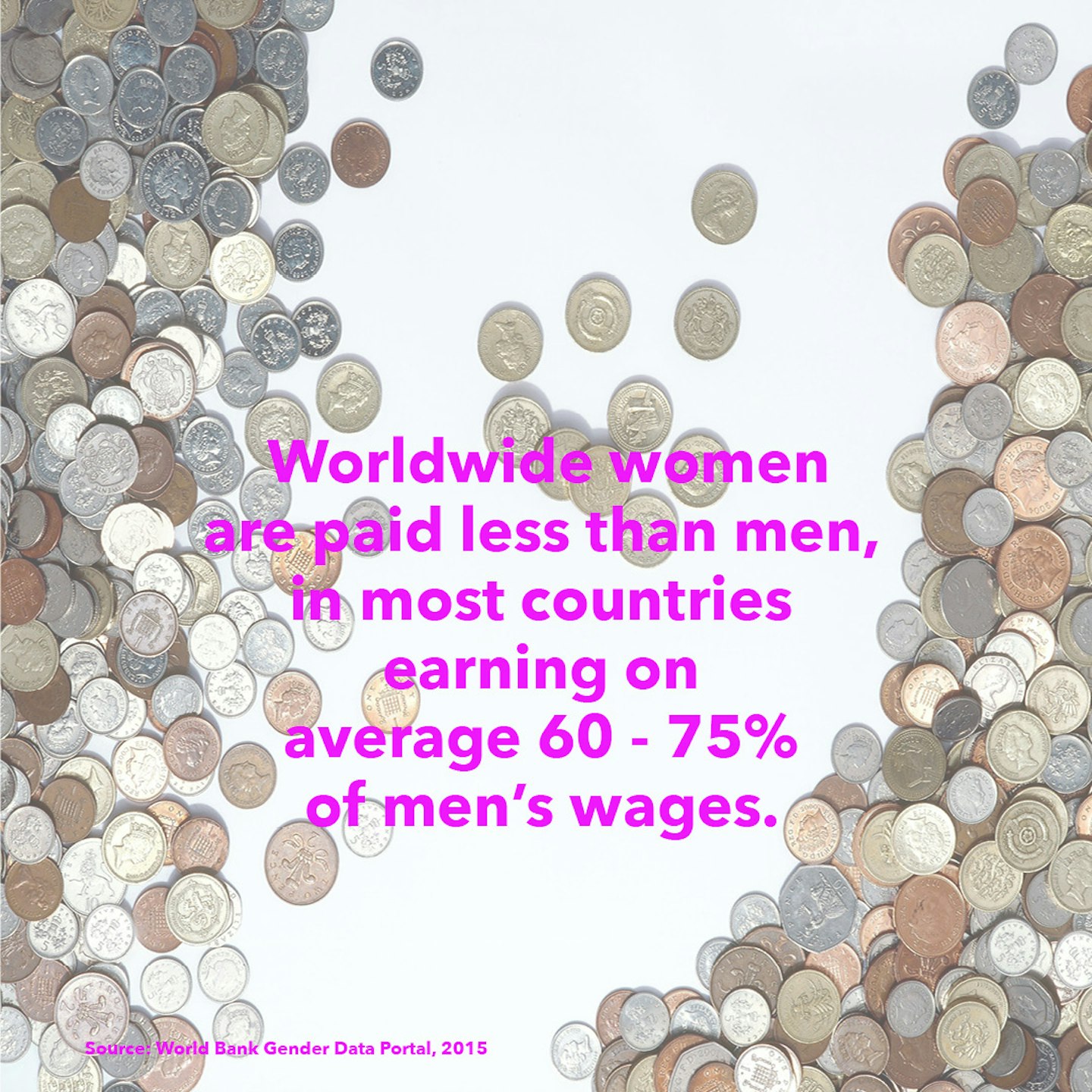
 2 of 18
2 of 18Facts about women around the world
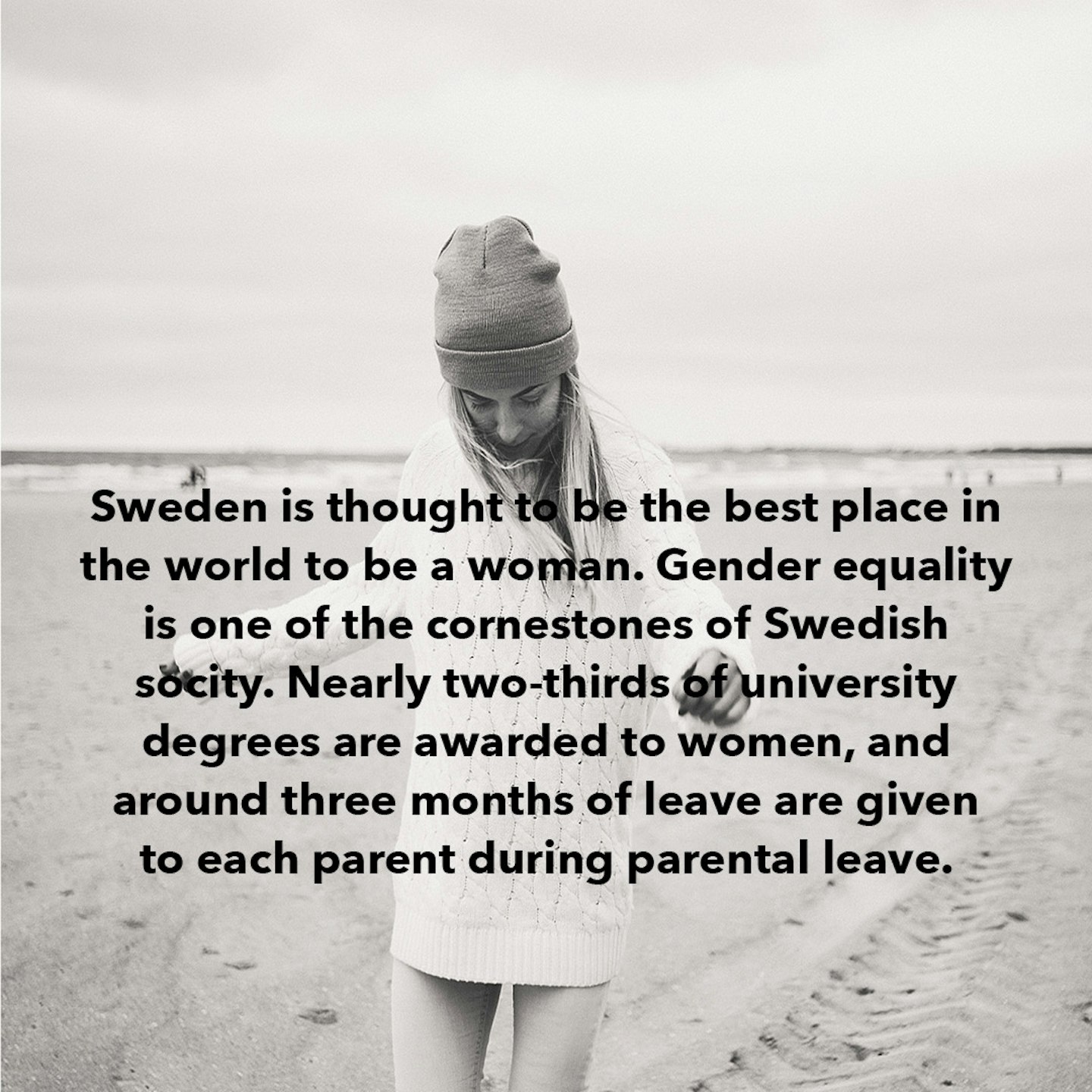
 3 of 18
3 of 18Facts about women around the world
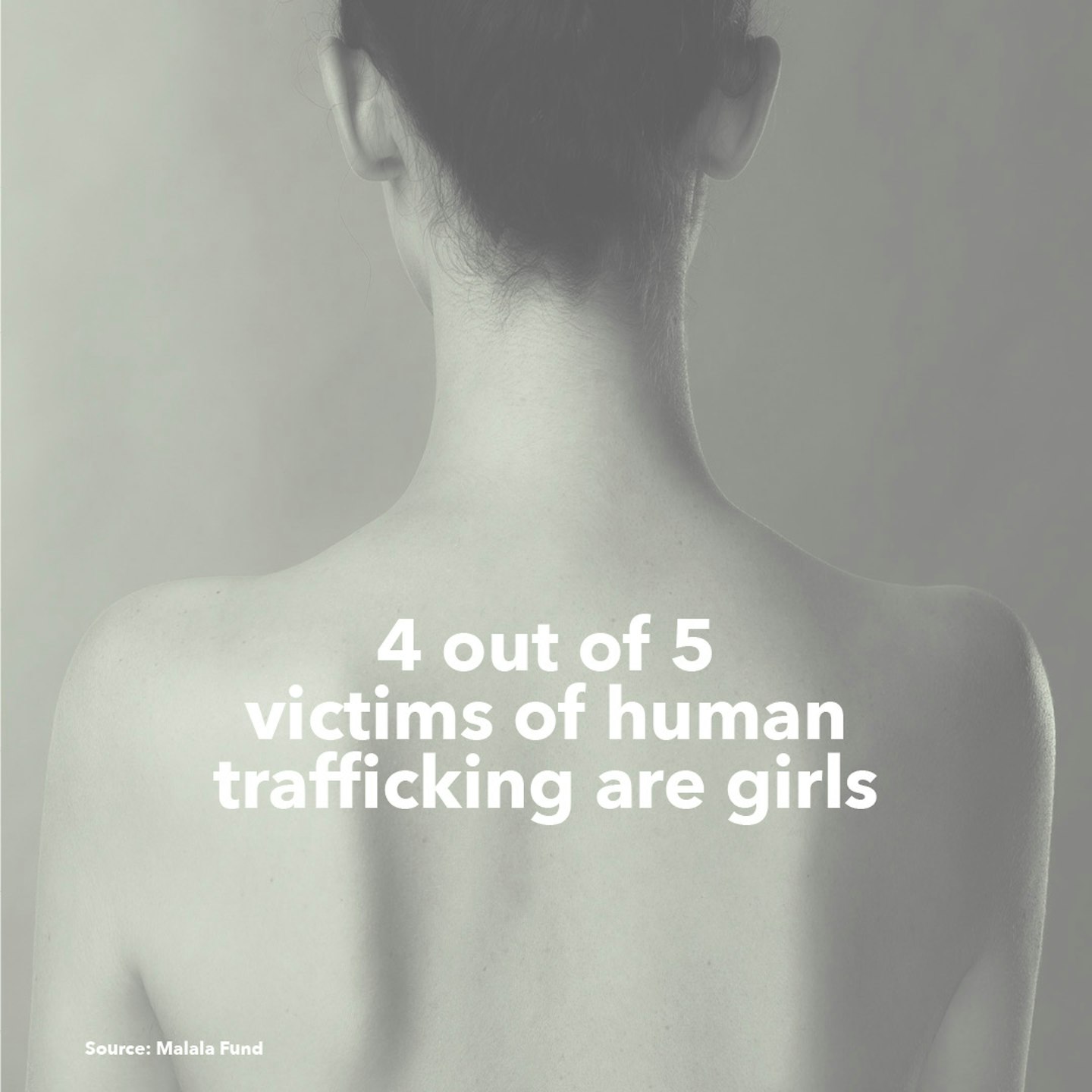
 4 of 18
4 of 18Facts about women around the world
 5 of 18
5 of 18Facts about women around the world
 6 of 18
6 of 18Facts about women around the world
 7 of 18
7 of 18Facts about women around the world
 8 of 18
8 of 18Facts about women around the world
 9 of 18
9 of 18Facts about women around the world
 10 of 18
10 of 18Facts about women around the world
 11 of 18
11 of 18Facts about women around the world
 12 of 18
12 of 18Facts about women around the world
 13 of 18
13 of 18Facts about women around the world
 14 of 18
14 of 18Facts about women around the world
 15 of 18
15 of 18Facts about women around the world
 16 of 18
16 of 18Facts about women around the world
 17 of 18
17 of 18Facts about women around the world
 18 of 18
18 of 18