‘Would you rather be anorexic or bulimic?’, a friend once asked me at school. Recalling the memory of being faced with this quite casually in the sixth form common room makes me really uncomfortable now. My twenty-five-year-old brain knows that it's an insensitive, inappropriate question, and so far from the ‘funny’ spectrum. But at the time it didn't. At the time, it was just two sixteen-year-old girls talking really frankly abouteating disorders.
I remember conditions like anorexia and bulimia being things that my generation of young women were explicitly aware of. I remember it being dangerously trendy to say you have an eating disorder and conversations about such would score you major points in the mental health buzzword lottery; much like anxiety does today.
And while the number of young women with eating disorders has long been a cause for deep concern, we're currently seeing a huge rise in admissions to hospital with potentially life-threatening diagnosis of the conditions, many of whom fall into this demographic .
Figures from NHS Digital obtained by the Guardian show that in the last six years, the number of people admitted with a primary or secondary diagnosis of an eating disorder has almost doubled. The number peaked at 13,885 last April while six years earlier in the 2010-11 bracket there were 7260 admissions. The number of women under the age of 19 admitted for anorexia rose from 1050 to 2025 in that period.
READ MORE: What Are The Best Natural Anti-Depressants?
Discover: Natural Anti Depressants
 1 of 11
1 of 11Omega 3
Omega-3 fatty acids are essential minerals which reduce inflammation and are vital to brain functions such as mood and memory. Your body doesn't produce them naturally so you can only get them in you via food (like fish, nuts and seeds) or dietary supplements.
 2 of 11
2 of 11Vitamin D
In addition to bone health, Vitamin D can play a vital role in the areas of the brain that are linked to the development of depression and other mental health problems.
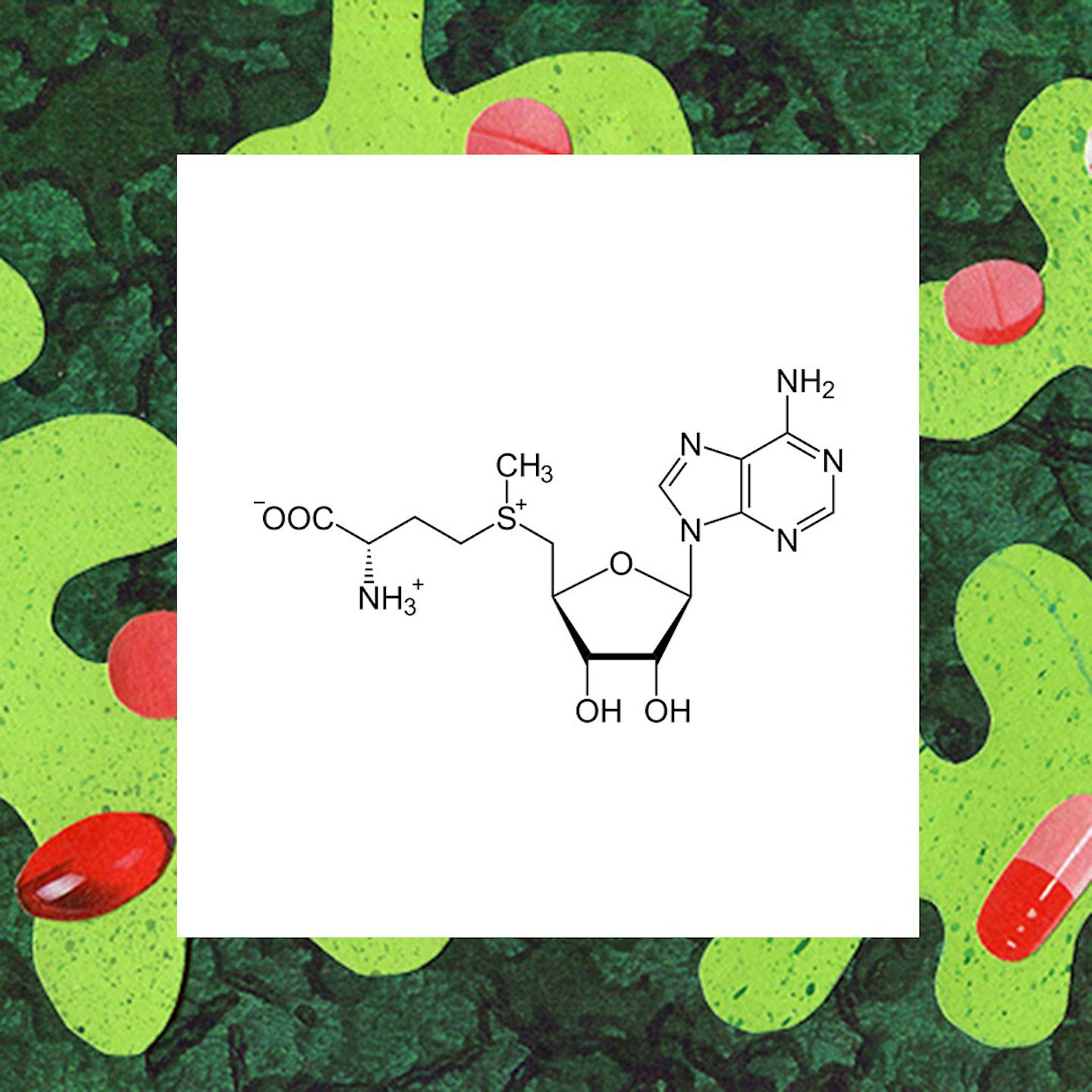 3 of 11
3 of 11S Adenosylemthionine
SAMeis a molecule that the body naturally forms and is available as a dietary supplement. In addition to depression and anxiety, it can be used for many other conditions including heart disease, fibromyalgia, tendonitis and many more. It is also recommended for PMS. It works by making sure that chemicals in the body that play a role in pain, depression, liver disease, and other conditions, actually do their job.
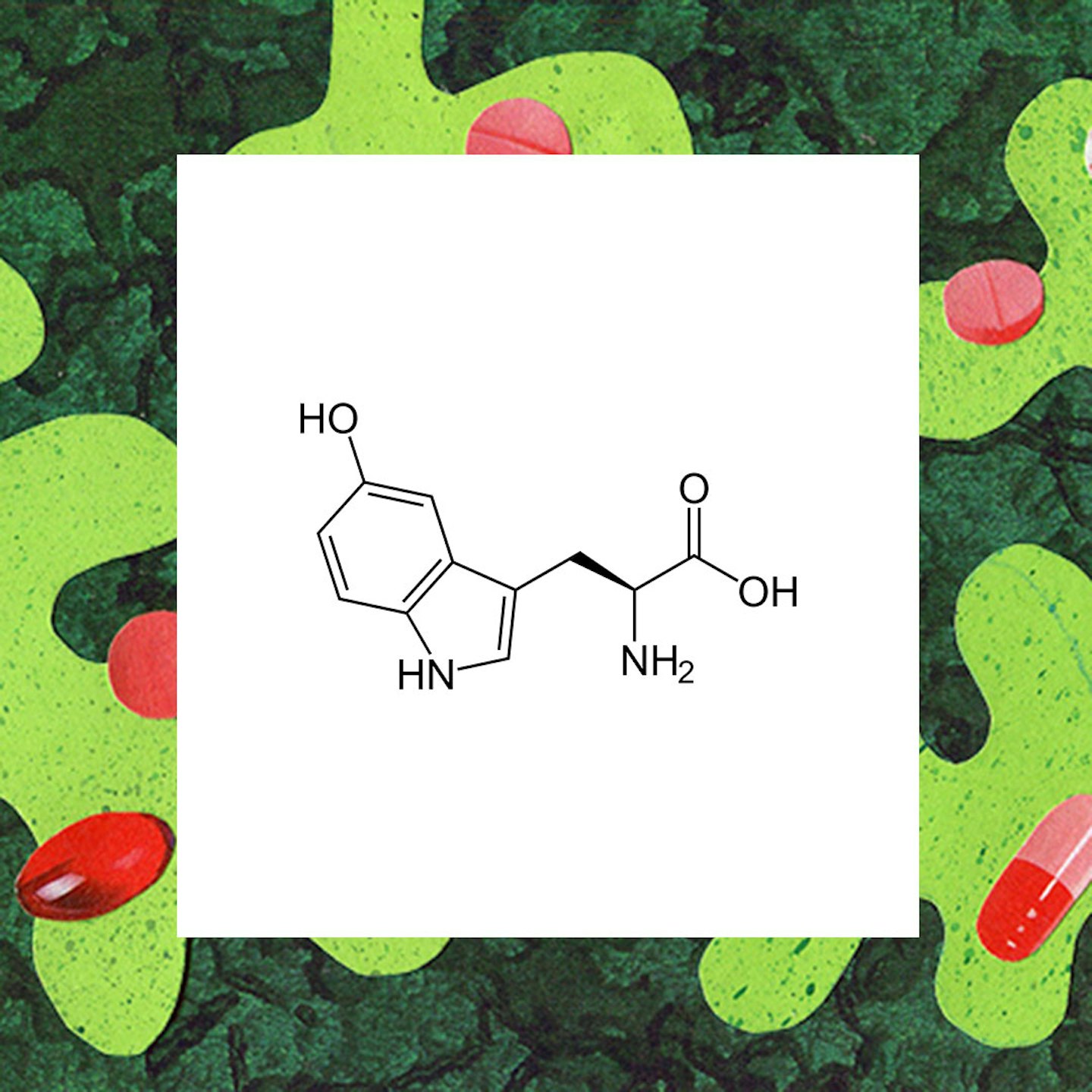 4 of 11
4 of 115-Hydroxytryptophan (5-HTP)
Like SAMe,5-HTP is also a chemical (an essential amino acid) that the body makes naturally. It works by helping to raise the serotonin (the happy hormone) levels in the brain. 5-HTP has been known to have a positive effect on sleep, mood, anxiety, appetite, and pain.
 5 of 11
5 of 11Roseroot Herb
A study conducted on whether the Rhodiola Rosea (Roseroot) herb was effective for depression showed that it was almost as effective as the popular antidepressant, Sertraline (Zoloft), but with fewer side effects. The herb boasts strengthening the nervous system, fighting depression, enhancing the immune system and memory, elevating stamina, aiding in weight-loss and increasing sexual function.
 6 of 11
6 of 11Iron
A lot of adults, especially women, suffer from iron deficiency, and guess what? Iron deficiency symptoms are pretty similar to depression symptoms, i.e. fatigue, irritability, and foggy brain. The recommended daily iron allowance in adults is roughly 8 to 18 mg daily (check with your doctor though because everyone's number is different).
 7 of 11
7 of 11Folate
If you don't have enough folate, antidepressants may not work. Some docs prescribe folate along with antidepressants to treat depression and improve the effectiveness the medication. Most adults need at least 0.4mg daily, which you can though food including dark leafy greens, beans and citrus fruit, or as a supplement.
 8 of 11
8 of 11B12
Vitamin B-12 and other B vitamins can play a role in producing mood-affecting brain chemicals and low levels of these may be linked to depression. If you have a poor diet and the body can not absorb enough B vits, your mood can be severely affected. Getting a blood test will determine how much of the B goodness you have in your system, and whether you need to stock up. B vitamins are found in animal products like milk, fish, meat and eggs, so if you are a vegan, you should definitely be getting your B's from dietary supplements and vitamins.
 9 of 11
9 of 11Zinc
Zinc is crucial to our system as it activates our digestive enzymes breaking down food, and helps prevent food allergies, which can avert depression. It also helps our DNA to produce and repair proteins, control inflammation and boost our immune system.
 10 of 11
10 of 11Tryptophan
Tryptophan is an essential amino acid which you get through food such as bananas, tamarind, oats, sesame seeds, kiwi and watermelon. Once in the body, it converts to niacin, serotonin and melatonin. Most antidepressants work by increasing the amount of serotonin in the brain and Tryptophan helps to increase serotonin levelswithout the extreme side effects of meds.
 11 of 11
11 of 11St John Wort
St John's Wort has been around for yonks and is one of the most popular natural methods used for dealing with stress, anxiety and depression. It's a plant with yellow flowers. There has been some scientific evidence that St. John's wort may be helpful in treating mild depression. It's been claimed that it works just like regular antidepressants in that it inhibits the reuptake of the neurotransmitters serotonin, norepinephrine, and dopamine.
It’s no secret that the conversation around mental health in the general sense has changed over this period of time. We’ve watched, listened and participated as it was anxiety and depression’s turn to earn societal understanding as reinforced by vocal celebrities and social media influencers. But at the same time and via the same means we’ve watched as movements like #cleaneating rose in popularity (before eventually being debunked a few times over) which can’t have helped our wider understandings of disordered eating in general.
UK eating disorder charity, Beat, also recently announced that calls to their helpline have also experienced a rapid surge and are likely to reach 17,000 by March 2018 (up by 7000 calls last year). Caroline Price, Beat’s director of services, told the Guardian suggested social media as one of the potential reasons for the sharp rise in people seeking – and not receiving – help for eating disorders.
‘Eating disorders are complex and there is no one particular factor that means you get one, but we feel eating disorders are on rise partly because of the challenges of today’s society’, she explained. ’This includes social media and exam pressure. They don’t cause eating disorders; someone will be predisposed to be the type of personality who will develop an eating disorder ... Then the challenges of social media and pressure to go to university all those things can compound so someone really does suffer with it’.
The nature of eating disorders has undoubtedly changed just as the world that they exist in has. But it also feels like our understanding of them and the support that’s required for those who suffer them is blocked by the elaborate rebranding of what problematic eating habits look like. In the last couple of years, they’ve been able to be disguised as a clean eating hashtag, as a quest for the perfect Revenge Body, or as a fleeting commitment to ditching gluten/dairy/meat from diets without properly promoting how to maintain a nutritious balance.
There are certainly many things that will have contributed to the sharp rise in hospital admissions. No thanks to the NHS's long suffering budgets and limited funding for mental health specifically. But it's clear that the systems in place are inadequate at the moment. There have been instances where people have had to have to relocate in search of sufficient community support. And if there's an increase in people reaching the level of severity that requires hospital services, doctors, MPs and campaigners have warned that something going seriously wrong in the interim at outpatients facilities and treatment centres.
If we're not there already, we can't be far from breaking point. And while steps absolutely need to be taken at early stages to prevent people becoming so severely unwell that a hospital stint is required, part of that process needs to be an overarching acknowledgment of the role social media plays in shaping the eating disorder playing field, because those conversations don't seem to be happening nearly as much as they should.
We've seen the positive that has come from the public conversations around depression and anxiety, and how these conversations have contributed to moving anxiety in the context of our digital lives now into mainstream acceptance. Now it's about time we did the same for eating disorders. No doubt it's difficult territory, but that's half the problem.
Follow Jazmin on Instagram @JazKopotsha
This article originally appeared on The Debrief.