Despite the fact that millions of women, all around the world, have been taking the contraceptive pill since its invention in the 1960s it seems many of us aren’t actually clear about how it works. It is the only drug regularly prescribed to healthy people. Millions of women in England alone take it dutifully, because it is one of the most effective ways to protect against unwanted pregnancy. Many of them find it works for well for them however, that isn’t the case for everyone…
We google ‘how the pill works’, ‘does the pill stop your period’, ‘is the pill safe’, ‘does the pill stop ovulation’ and ‘is the pill bad for you’, ‘can the pill make you gain weight’, ‘side effects of the pill’, ‘can the pill make you tired’ and ‘can the pill cause depression’ in our thousands.
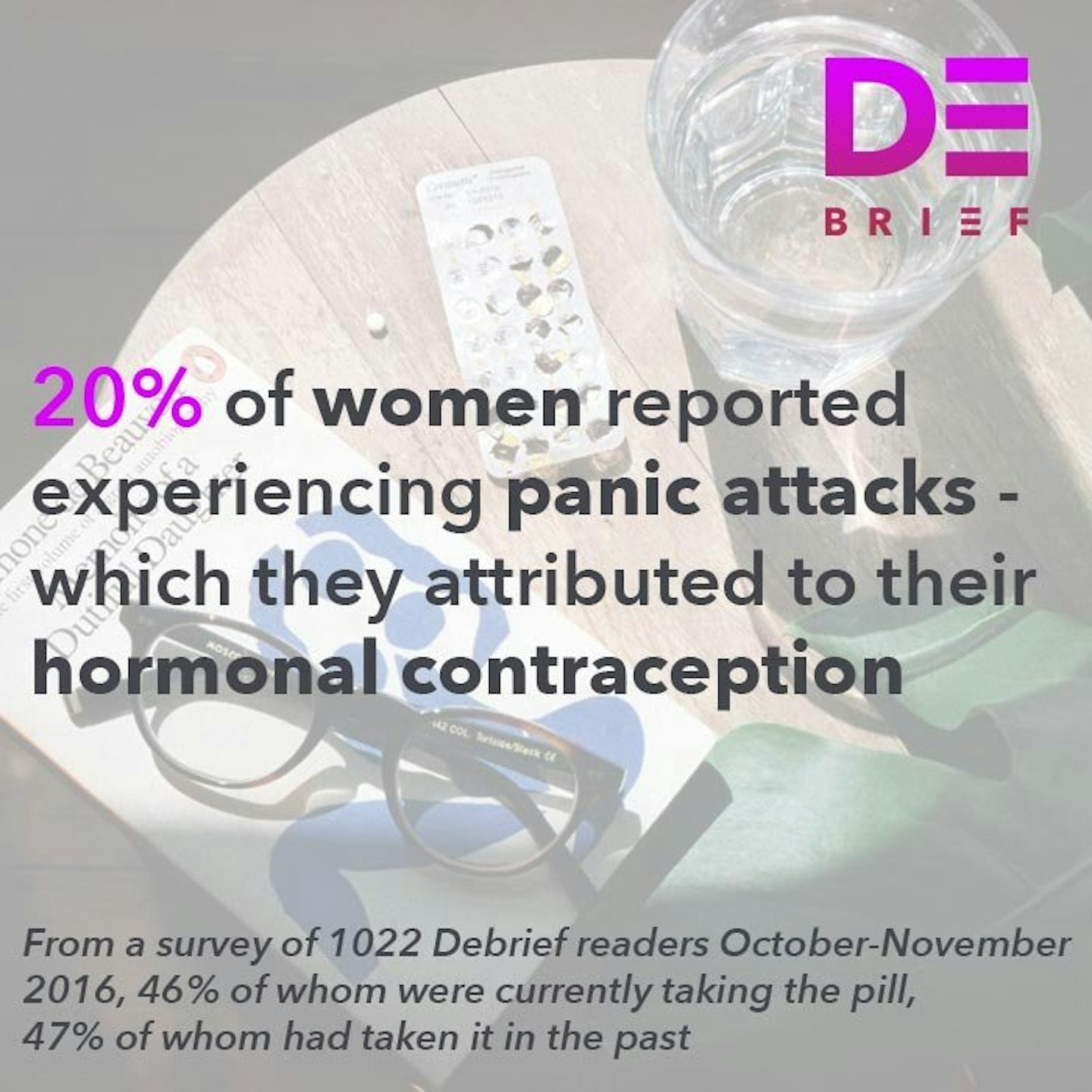
Perhaps the real question is this: why are we asking google questions about a medication that so many of us take, every day, for a large proportion of our lives? The Debrief have conducted an in depth investigation, Mad About The Pill, which involved submitting freedom of information requests (FOI) to the NHS as well as a survey of over a thousand women. One of the recurring themes, which came up over and over again, when we spoke to the women who responded to our survey was that they had received mixed messages, different information and inconsistent treatment from medical professionals.
We spoke to three experts as part of Mad About The Pill. We asked them how the hormones in the pill work and, specifically, how hormonal contraception can interact with a woman’s mental health (for better and for worse) …
Professor Anne MacGregor
Professor MacGregor is a specialist in Sexual and Reproductive Healthcare at Barts Sexual Health Centre in London. She co-authored* The Pill* which is a definitive work on reproductive health. She also refined what’s known as ‘the pill ladder’. You might have seen it, it’s a handbook which lists every pill and its contents, some GPs will consult in when trying to decide which pill will work best for you.
She says: ‘It’s important to open any discussion on the pill in the context of contraception in the context of it as one of a number of different methods. Much of what I and my colleagues do, is about trying to tailor the method of contraception to the individual rather than the other way round.’
Dr Tamsin Lewis
Dr Lewis specialises in bio-identical hormone therapy at the Marion Gluck clinic in London.
She says the issues surrounding the contraceptive pill are, at their core, about ‘patient empowerment’. ‘It will take a big public health mission to change people’s thinking.’
Professor John Studd
Professor Studd is a consultantgynaecologist at the Chelsea & Westminster Hospital, London and a professor of gynaecology at Imperial College. He started the first menopause clinic in Europe and has studied the effects of hormones on mood, depression and libido.
He says ‘female hormones have a profound effect on mental health’
How does the contraceptive pill * actually * work?
Right now, throughout your body, tiny chemical messengers are travelling around. They coordinate pretty important things like growth, your metabolism and your fertility. They also influence other major stuff, you know, like how your immune system works, your moods and your behaviour. I am, of course, talking about hormones.
Hormones aren’t generally given the credit their due. Women are so often described as being ‘hormonal’ which is, almost always, a negative thing if not an outright insult which in no way takes into account the mind blowing complexity of our endocrine systems. Because of hormones human beings can convert what we eat into energy which powers our bodies, create and give birth to new life and go through puberty. It’s hormones that power our ‘flight or fight’ adrenaline response to threats and stress, because of them we escaped sabre tooth tigers and made it through the early stages of our evolution.
The endocrine system, by the way, is the system of glands which store hormones and, on the brain’s command, send the right chemical into your blood stream at the right time. Your ovaries are an endocrine gland.
Professor MacGregor says:
‘Most of the pills contain synthetic hormones – but we have two new pills now which contain exactly the same oestrogen as you find in your ovaries and that – as we move on – is where the development is going to try to make the hormones equivalent to your own hormones so it is much more natural in that sense. However, right now, the majority of them contain a synthetic oestrogen and a synthetic progesterone – which are, in a way, to replace your own natural oestrogen and progesterone. They work to switch off your menstrual cycle and basically allow your ovaries to sleep while you’re taking the hormones so you’re not releasing an egg every month and can’t get pregnant – and then when you stop taking the pill the ovaries wake up again.’
The process by which it all happens is pretty complex but, in an eggshell, it goes something like this:
-Synthetic oestrogen stops your pituitary gland from producing the hormones with make your ovaries release an egg
-Synthetic progestin also stops your pituitary gland releasing an egg and thickens your cervical mucus to make it really difficult for sperm to get from there to an egg.

So, is it true that taking the pill interrupts your natural hormonal cycles and mimics pregnancy?
Professor MacGregor says:
‘Well, it’s mimicking pregnancy in the sense of that it’s stopping you ovulating which is exactly what happens when you’re pregnant – in that sense yes, it’s preventing you from being pregnant by putting the body in its natural contraceptive state which is to prevent pregnancy while pregnancy is occurring.’
Can you tell us more about contraceptive pills that contain natural as opposed to synthetic hormones?
Professor MacGregor says:
‘They’re called Zoely and Qlaira. This is something that has been in development for years but has been difficult to develop because you can get quite an erratic bleeding pattern which as you can imagine women don’t want to experience. With Qlaira they’ve managed to do it by creating multiple dose changes. With Zoely they’ve managed to use effective progestins and lower levels of oestrogen which are similar to those which your body naturally produces throughout the menstrual cycle.’
Are there benefits of using natural as opposed to synthetic hormones?
Professor MacGregor says:
‘Yes and no – the concern with the combined pill, and I should say that its become less of a concern as the levels of the hormone in the pill have reduced – 20-30 micrograms as opposed to 100-150 microgram when it first came out. However, there is still the concern that because it makes your blood a little bit stickier that if you have a genetic predisposition to blood clots then you’re just slightly increasing that risk – so it’s a low risk but its still a risk –that’s the reason why we’re very careful as people who are giving the pill to women to ensure that the benefits of taking the pill to that particular person outweigh the risks which, for most women, they do.’
Professor Studd says:
‘There is good evidence now that there is a 30% increase in depression in women having the combined pill but there is a 100% increase in depression in women having the progesterone-only pill. What happens is that women are by-and-large intolerant, sensitive to the progesterone and more so synthetic progesterone. By-and-large women like oestrogen. But progesterone is bad news for them.’
Why do some women respond badly to progestrogen/progesterone?
Professor Studd says:
‘It’s very hard to be certain about it but, the fact is, that these women don’t like progestrogen because some changes in their neurotransmitter system, whether it’s serotonin, dopamine or whether it’s a genetic change. There’s some recent work showing that the genes are different in women who don’t like progesterone and that’s as far as we can go scientifically. But the facts are quite clear – that depression is more common on the pill, the combined pill, and much more common on the progesterone-only pill.’
How do hormone levels affect a woman’s body?
Professor MacGregor says:
‘The way that the endocrine system works is that no hormone works in isolation. They interact with other hormones. For example, there’s an interaction with levels of oestrogen and serotonin – which is a factor in migraines, but it’s also your happy hormone. In very simplistic terms – if your oestrogen levels are dropping and your serotonin levels are dropping in parallel then its going to affect your mood – and it is then going to be modified by other hormone changes. It’s a very complicated system suffice to say – there’s a knock on effect with the other hormones. Our understanding of how the pill can affect migraine and also mood is something that’s increased in recent years but potentially wasn’t at the forefront of people’s minds when the pill was first conceived.’
Can you explain why some women experience negative mental health side effects while others don’t?
Dr Lewis says:
‘The thinking on this is that all women are different: they have different hormone levels as their base line. Because the pill itself because stops ovulation, it can stabilise hormone levels – and actually improve things for some people. In my experience, in those who have a predisposition to mental health problems (and we should take into account that the research is now there to tell us that the pill may change people’s behaviours in terms of the relationships they seek for instance and their food cravings which may exacerbate moods etc.) it can worsen mood swings. Then there’s the negative side effects of very synthetic hormones - like in the pill - and I think there’s a lack of understanding and awareness about the differences between synthetic hormones and bio identical hormones – which are very much a -low risk intervention when you compare them to synthetic hormones as found in the contraceptive pill. In the medical profession people do not know that there’s a big difference between them – progestins and natural progesterone – but in the fertility world and the world of gynaecology people hugely recognise that there’s a difference.’
What do you think the future holds for hormones in contraception?
Professor Studd says:
‘We do know, from work on the menopause and hormone replacement therapy (HRT), that transdermal hormones are safer than oral hormones. There is no question about that. So, when going onto HRT, women should have transdermal hormones and not oral hormones. Unfortunately, that’s not available on the market for contraception because the transdermal hormones would be weaker. We’d have to do a huge amount of work, costing a huge amount of money, to get this right. But, in the future, I have no doubt that we will see the end of oral synthetic oestrogens and oral synthetic progestrogens. There will be a way of getting the dose right, the combination right of transdermal oestrogens and natural progesterone for contraception. The way synthetic oral hormones are prescribed [in contraception] is pretty rudimentary now to be honest but what it is that causes depression in women having progesterone or progestrogen we don’t know.’
Professor MacGregor says:
‘There are, I think, about 40 different varieties by the time you juggle different types of progestrogen and different types of doses. And a woman will respond to each of those different pills in a slightly different way. But that is only the beginning of the story because there is a very clear need to try and make pills as safe as we possibly can, to consider whether actually having them in a pill form is the most appropriate route.’
The link between hormones and mental health is a well established one. It is known that a potential side effect of hormonal contraception is mental health problems. Hormones are complex, we still don’t understand them fully, nor do we understand mental health fully.
However, what’s clear is that it’s time for further progress and innovation when it comes to contraception and reproductive health. The knowledge and expertise are out there, it’s within our grasp. We innovate in other areas of medicine and technology every day so why not contraception? Let’s face it, not matter how many people tell you natural ‘family planning’ and withdrawal methods work it’s not really a solution we can all feel confident in.
The more you look into this the more Gloria Steinem’s essay* If Men Could Menstruate *seems more pertinent than ever. If men could menstruate, she wrote in 1978, ‘to prevent monthly work loss among the powerful, Congress would fund a National Institute of Dysmenorrhea. Doctors would research little about heart attacks, from which men would be hormonally protected, but everything about cramps.’
If you are concerned about your pill, or hormonal contraception, please contact your GP immediately
***Share your pill stories with us @thedebrief#madaboutthepill ***
You might also be interested in:
Follow Vicky on Twitter @Victoria_Spratt
This article originally appeared on The Debrief.
