One of the most shocking headlines from Britney Spears' testimony is news that her conservators have been forcing her to use an IUD to stop her getting pregnant. Britney testified to an LA courtroom yesterday, saying 'I have an IUD in my body right now that won’t let me have a baby and my conservators won’t let me go to the doctor to take it out.
IUD meaning
Intrauterine Device or ‘Copper Coil’ (IUD)
What is an IUD?
So, what is an IUD? It's a T-shaped plastic and copper device inserted into the womb by a doctor or nurse and lasting 5-10 years (depending on the type). Copper works similarly to progestogen, thickening cervical fluid and thinning womb lining.
Britney has said she didn't want to have the IUD and hoped to have a baby with her boyfriend Sam Asghari. But for those who want to know more about the different birth control methods, here's a comprehensive guide to IUDs and all your other contraception options....
For many of us, finding ‘the right method of contraception’ is a long-standing game of trial and error, interspersed by break-outs, bloating, and evenings spent sobbing inconsolably at, well, everything. While figures show that nine out of 10 women using contraception are on the pill – making it the top choice with 3.1 million users – more of us than ever are questioning our birth control. Perhaps it’s down to the launch of books like How the Pill Changes Everything: Your Brain on Birth Control, or maybe the rise of health-conscious millennials, questioning what we’re actually putting in our bodies. Now, we want to understand_all_of our options. But when 10-minute GP appointments don’t allow for such a thorough explanation, where do we turn?
Enter The LowDown – the ‘Trip Advisor for contraception’ – a first-of-its-kind review platform. Now with 10,000 monthly visitors, users submit anonymous reviews for different contraceptive methods. 'In my search for the right method, I realised I couldn’t find useful data on real women’s experiences,' explains founder Alice Pelton, 31, of its origin. 'Your options? Speak to friends, doctors, or read intimidating internet forums. These are small sample sizes, and you’re never sure whether one person’s experience is the norm or the exception. I wanted to give women a deeper understanding of their options.'
But as Alice puts it, there are no ‘five-star’ methods, and women are desperate for new options that offer fewer side effects. It’s why ‘the male pill’ – trials were halted in 2016 when 20 participants complained of side effects – made headlines. 'Pharmas assume women have "enough methods", but as all hormonal contraceptives contain variations of the same hormones, there actually isn’t much choice,' says Alice. 'I want to see more funding into development of new methods for both sexes. After years of battling with contraception, it’s the least women deserve.'
Until then, getting to grips with all types of birth control can seem pretty overwhelming. So, here’s the Grazia guide to all contraceptive methods available on the NHS, all 92-99% effective if used correctly...
Hormonal Methods Of Contraception
Hormonal methods all work in the same way, but are just administered differently. Some are ‘combined’ (using both oestrogen and progestogen); while others are progestogen-only. ‘Combined’ methods prevent pregnancy in three ways: stopping ovulation; thickening the fluid in your cervix to prevent sperm entering the womb; thinning the womb lining to prevent an embryo growing. Progestogen-only methods don’t stop ovulation, but are just as effective.
Combined Pill
The pill contains both oestrogen and progesterone, and is a small tablet taken daily. The time window depends on the type – there are over 20 types ofcombined pill. Side effects can include acne, headaches and tender breasts. 'The pill is often offered when a women starts having sex, which is sensible, so she can understand how her body tolerates hormones,' says Alice. 'But there isn’t enough focus afterwards to check on side effects – it’s how women get stuck on the pill.'
Progestogen-Only Pill (‘Mini Pill’)
Unlike the combined pill, the mini pill only contains progestogen. Some mini pills contain desogestrel, which can also stop ovulation. You swallow one tablet each day (three-hour window for traditional mini pill; 12-hour window for desogestrel pill). The mini pill is recommended for those who should avoid oestrogen, such as migraine sufferers.
Contraceptive Implant
A small, flexible plastic rod, placed under the skin in your upper arm, that releases progestogen. It’s inserted by a doctor or nurse, lasts for three years, and can be professionally removed at any time. The most common side effect reported on The Lowdown is spots/ acne.
Contraceptive Injection
An injection by a doctor or nurse, which steadily releases progestogen. It lasts for 8-13 weeks (depending on the type) before needing a top-up. The most common side effect on The Lowdown is headaches.
Contraceptive Patch
A beige plaster that releases oestrogen and progestogen. You stick it anywhere on the body (except breasts, sore/ irritated skin, or an area easily rubbed off) and change to a new patch every seven days. Can be worn in the the bath or swimming pool.
Intrauterine System or ‘Hormonal Coil’ (IUS)
T-shaped plastic device inserted into the womb by a doctor or nurse, releasing progestogen and lasting 3-5 years (depending on type). 'This method currently has the highest satisfaction rating, at 3.7 out of 5,' says Alice. 'Reviews report no negative impact on mood or reduction in sex drive – perhaps because the hormones are administered locally into the womb. Plus, periods stopped in 57% of users, and made them lighter for 24%. Many say the discomfort of getting it fitted is "worth it".'
Vaginal Ring
Plastic ring which you place inside your vagina, releasing oestrogen and progestogen. It lasts a month, and it can’t ‘get lost’. Sometimes it can fall out – if it’s more than three hours, use additional contraception
Non-Hormonal Methods Of Contraception
Non-hormonal birth control usually works by stopping sperm from ever reaching the egg in the first place (often called ‘barrier methods’), and are associated with fewer symptoms than hormonal methods. The downside is that they can be more fiddly, costly (as most are one-time uses), or are permanent.
Caps/ Diaphragms
Silicone circular dome with spermicide inserted into the vagina before sex. It covers the cervix so sperm can’t get through and must be left for at least six hours after sex. More spermicide is required if you have sex again within six hours, or if you inserted it three or more hours before sex.
Male Condoms
Commonly-used latex or polyurethane sheaths that are worn on the penis and stop sperm getting to the womb. Also protect against STIs.
Female Condoms
Plastic pouches that are worn inside the vagina and stop sperm getting to the womb. Also protect against STIs.
Intrauterine Device or ‘Copper Coil’ (IUD)
As we said earlier, it's a T-shaped plastic and copper device inserted into the womb by a doctor or nurse and lasting 5-10 years (depending on the type). Copper works similarly to progestogen, thickening cervical fluid and thinning womb lining.
Sterilisation
Permanent surgical procedures: fallopian tubes are blocked/ sealed in women, so embryos cannot be carried from ovaries to the womb; for men, the tubes that carry sperm are cut/ sealed (vasectomy).
Natural Family Planning (‘Fertility Awareness’ or ‘Rhythm Method’)
Monitoring fertility signals during your cycle to determine when you’re fertile, and using protection during those times. Signals include: cycle length; daily body temperature readings; changes to cervical mucus. It can take 3-6 months to get the hang of this method, but “it’s increasing in popularity,” says Alice. For example, the Natural Cycles app is a newly-FDA-approved method of contraception, claiming to minimise human error as the algorithm interprets fertility for you. But this is a new, and therefore under-studied, method of birth control, and we advise you really research Natural Family Planning before going ahead.
The jury is out on whether condoms decompose, but some brands are getting conscious with their condoms…
Planet-Protecting Protection
 1 of 3
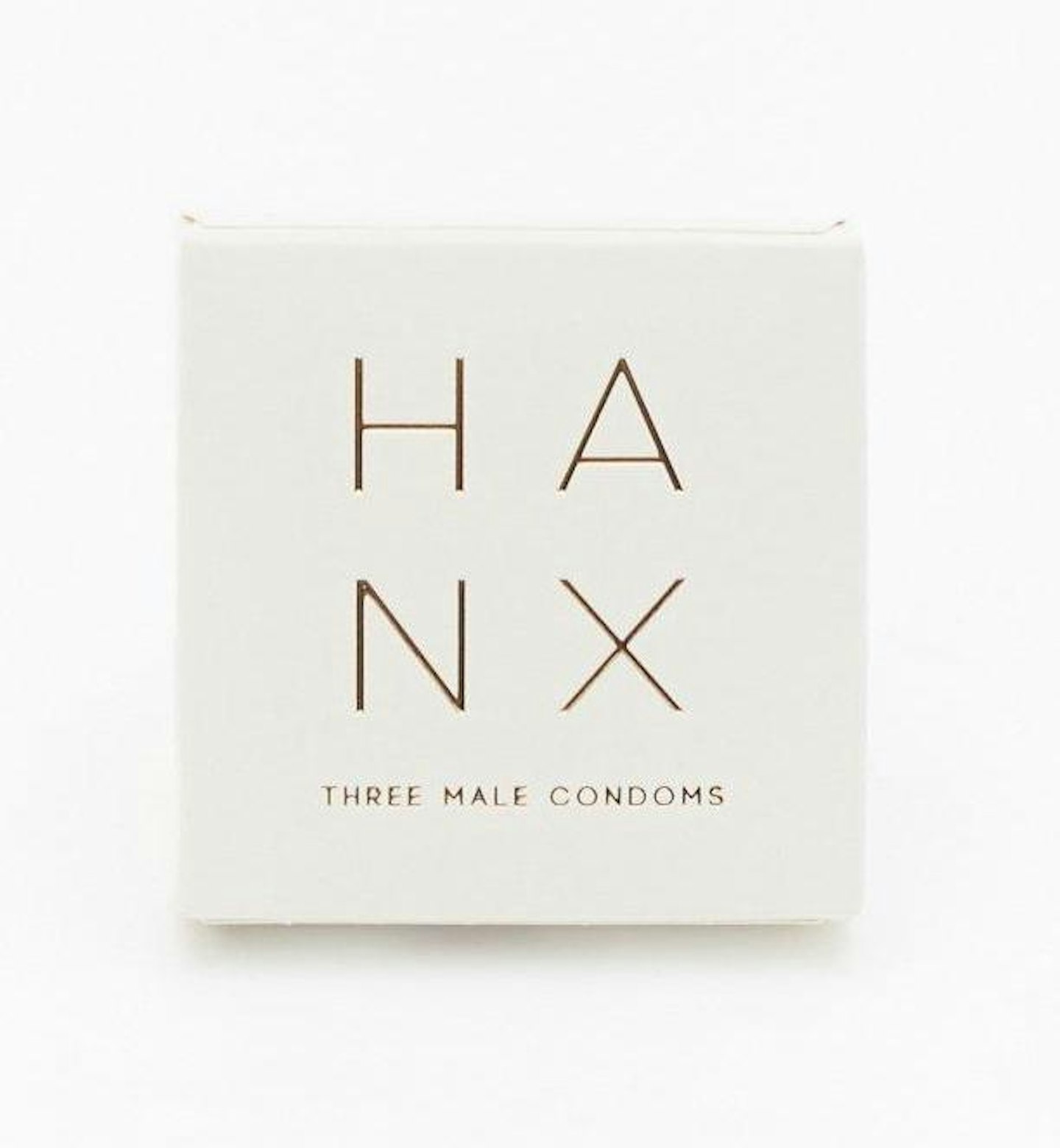
1 of 3HANX Condoms, £16.99 for 10
100% natural, biodegradable latex, vegan and ultra-thin, too.
 2 of 3
2 of 3Einhorn Fairstainable Vegan Condoms, £9.49 for 7
Focused on sustainable and ethically sourced rubber and recyclable paper bags.
 3 of 3
3 of 3Sustain Natural Condoms, £5 for 3
Vegan, non-GMO, fair-trade latex, plus 10% of profits go to women's healthcare organisations.
